AHVLA Report: Porcine Reproductive and Respiratory Syndrome
UK - The Animal Health Veterinary Laboratories Agency (AHVLA) has looked into Staphylococcal skin disease causes skin lesions resembling pig pox and porcine reproductive and respiratory syndrome (PRRS) underlying finisher disease and mortality, according to its Pig Disease Surveillance Monthly Report for September 2014.Porcine Reproductive and Respiratory Syndrome Disease Alert
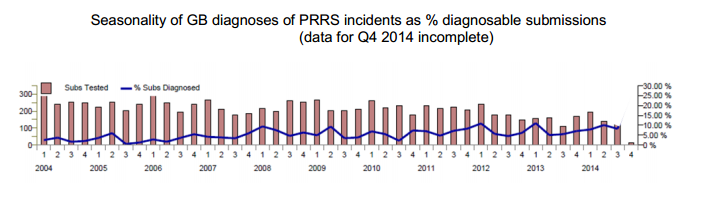
Trend analysis of the seasonality of GB porcine respiratory and reproductive syndrome (PRRS) over recent years shows that there tends to be a peak in diagnoses in the winter months as illustrated in the figure below.
This probably reflects the fact that climatic conditions over the winter tend to favour survival of PRRS virus and promote transmission.
Survival of the virus in contaminated pig accommodation, vehicles or on other fomites is also more likely as effective cleaning and disinfection and drying of surfaces is harder to achieve in wet and cold weather.
This year, the diagnostic rate of PRRS during July to September was higher than the same quarter in any of the last 10 years. This raises concern that there will be more active infection present going into the cooler months, further increasing the risk of virus spread during this time.
Obtaining an accurate diagnosis in respiratory disease outbreaks assists in determining whether PRRS virus is involved and in deciding on specific control measures.
Outbreaks of respiratory disease may involve more than one infectious cause and, ideally, a batch of three typically affected pigs early in the course of disease should be sampled or submitted to provide the best material for both diagnosis and pig disease surveillance.
 Reproductive Disease
Reproductive Disease
Evidence of recent exposure to Leptospira Bratislava in sows returning to service
Blood samples were submitted for serology from sows on two separate breeder-finisher units under the same ownership, when a high number of returns to service occurred. Serology using the microagglutination test (MAT) for Leptospira Bratislava revealed the majority of the sows tested to have titres in excess of 1:400, with some as high as 1:12800.
MAT titres of 1:400 or more in unvaccinated pigs are suggestive of recent leptospiral infection. No other details were available but pigs, rodents and some other wildlife are hosts for L. Bratislava which is the leptospire serovar to which antibodies are most commonly detected in the GB pig population.
Opinion is divided regarding the significance of the role that L. Bratislava plays in infertility in sows.
Alimentary Disease
Incidents of clostridial enterotoxaemia continue in neonatal pigs
Clostridial enterotoxaemia was diagnosed by Bury St Edmunds as the cause of diarrhoea and deaths in neonatal piglets.The problem was occurring on a recently established outdoor weaner-producer commercial herd of 1000 sows. Sixty five of 140 litters were affected in the farrowing batch and this was the second batch to have been involved.
A poor response to antimicrobial treatment was described and mortality had increased significantly to 26 per cent. About three-four piglets showed signs in affected litters with a creamy yellow scour starting around five-days-old after which piglets wasted, whilst a few piglets were dying without any prior clinical signs.
Four dead untreated piglets were submitted in which there was a necrotic enteritis particularly affecting the jejunum.The piglets had dull tacky subcutaneous tissues and accumulations of cream-white material in the kidney pelvises consistent with dehydration.
Clostridium perfringens toxin testing revealed alpha and beta toxins in small intestinal contents from one piglet (pointing to Cl. perfringens type C) and alpha toxin only in two others.
No other neonatal enteropathogens were identified although involvement of coccidiosis could not be fully investigated as the piglets were too autolysed for intestinal histopathology. No porcine epidemic diarrhoea virus was detected by PCR.
Necrotic intestinal lesions due to Lawsonia intracellularis on two units
Wasting was the main clinical sign reported in a group of 15-week-old pigs and three were submitted to Penrith for investigation. Necrotising typhlocolitis was found in all three pig. No Salmonella was isolated and histopathology revealed changes consistent with porcine proliferative enteropathy with special stains showing intra-epithelial small bacteria consistent with Lawsonia intracellularis.
This form of disease due to L. intracellularis usually causes the most prominent lesions in the small intestine but they can extend into the large intestine, as in this case and resemble those seen in salmonellosis.
On a second unit, a small group of 16-week-old pigs were affected with acute onset haemorrhagic diarrhoea and poor growth and post-mortem examination was arranged with the Royal Veterinary College under the new arrangements for external post-mortem examination provision with APHA.
In one of the pigs which was euthanased and submitted, there was severe necrotising and haemorrhagic enteritis with crumbly yellow material in small intestinal contents. No Brachyspira or Salmonella species were isolated but histopathology confirmed a proliferative enteropathy due to Lawsonia intracellularis.
Bowel oedema after arrival of pigs at their finisher site
Increased mortality in 10-week-old pigs recently-arrived from the breeding premises led to submission of four dead pigs to Penrith for post-mortem examination.
There had been 10 deaths and a further 15 pigs were affected with swollen eyelids, ataxia, hindlimb weakness and rapid death in the batch of 550. Cases did not respond to treatment with penicillin.
The pigs were vaccinated against Mycoplasma hyopneumoniae and PCV2 at source and were fed a commercial ration containing amoxicillin for the first 10 days after arrival before switching onto unmedicated ration.
The four pigs submitted were below target weight for age ranging from 13kg to 25kg and two appeared hairy and pale with watery blood, although iron deficiency was not present. Gross lesions were minimal with reddening of mesenteric lymph nodes and meningeal congestion.
Haemolytic Escherichia coli isolated from the ileum was typed as strain E4; serotype O139:K82 which is a serotype associated with bowel oedema in pigs, confirming this diagnosis. The E. coli isolate showed in vitro resistance to apramycin, spectinomycin, trimethoprim/sulphamethoxazole, ampicillin and tetracycline the in-feed antimicrobial may have favoured better survival of this pathogen relative to other intestinal commensals.
Potential issues at the source unit were considered worth investigating given the uneven bodyweights of the pigs.
Respiratory Diseases
Porcine reproductive and respiratory syndrome underlying finisher disease and mortality
Pigs were submitted to Thirsk from a nursery-finisher unit, with problems in 50-60kg pigs that started to fade, then became pale and died.
No obvious enteric or respiratory signs were detected. Pigs were vaccinated against Mycoplasma hyopneumoniae and PCV2. Post-mortem examination revealed varying degrees of peritonitis, pleuritis and pneumonia.
PRRSv, Mycoplasma hyorhinis and M. hyoneumoniae were all detected by PCR, and Trueperella pyogenes was isolated from the pleura of one pig. Histopathology revealed interstitial pneumonias consistent with PRRS and some milder changes consistent with possible mycoplasmal infection.
The lesions were fairly chronic in these pigs and the earlier involvement of Haemophilus parasuis or other pathogens cannot be ruled out.
Bacterial meningitis, pneumonia and streptococcal endocarditis in a finisher
A 15-week-old pig was submitted to Sutton Bonington to aid investigation of respiratory signs, diarrhoea and weight loss in the finishing group.
The clinical disease had begun from six to eight-weeks-old with 10-15 per cent of pigs affected. In the submitted pig, there was meningitis associated with Streptococcus suis type two and a bronchopneumonia associated with Pasteurella multocida, Mycoplasma hyopneumoniae and Mycoplasma hyorhinis.
There was also a vegetative endocarditis associated with a group L Streptococcus species infection. Given the presence of multiple bacterial pathogens and older age that this pig was submitted, it is possible that the disease which had occurred earlier in rear had involved viral infection.
Systemic Disease
Mulberry heart disease diagnosed causing sudden death
A nine-week-old housed pig dying suddenly was submitted from a group of 2000 to investigate five deaths over the preceding few days. Pigs were found dead or were dying after being found paddling in lateral recumbency in a herd considered free of Streptococcus suis type two.
There was skin reddening, fibrin stranding and a moderate excess of fluid in pleural and pericardial cavities, and mild interlobular pulmonary oedema. Together with brush-stroke haemorrhages over the epi- and endo-cardium of the chambers of the heart, these findings were suggestive of mulberry heart disease (MHD).
This was confirmed by histopathology which revealed severe necrotising myocarditis and liver congestion likely to reflect the heart failure. No S. suis of other bacterial pathogens were isolated but in view of the nervous signs occurring in some pigs, brain histopathology was also undertaken as a precaution and no significant lesions were present.
MHD is related to vitamin E and/or selenium imbalance, and further investigation can include testing bloods from pigs in the same cohort as pigs which were affected with MHD for selenium and vitamin E.
Nervous disease
Water deprivation after weaning and moving outdoors
Water deprivation was diagnosed in two combined litters of recently weaned 12-week-old pigs which had been moved to an outdoor pen. Four days after moving at least nine of the group of 16 pigs developed nervous signs including blindness, ataxia, aimless wandering and rapid respiratory rate after a short period of malaise and anorexia.
These signs are typical for salt toxicity. Four died and were submitted to Bristol University for post-mortem examination under the new arrangements for external post-mortem examination provision with APHA.
Findings included dry stomach contents and tacky sub-cutaneous tissues indicating dehydration. There was no evidence of bacterial meningitis from cultures and salt toxicity/water deprivation was confirmed by brain histopathology with mid-laminar cerebral cortical neuronal necrosis detected in the parietal and temporal cortex.
There was no obvious reason why this had occurred but advice was given to ensure access to adequate fresh drinking water at all times, it is possible that the recent move meant that pigs had not found the water bowl or that there had been some temporary interruption to supply.
Musculoskeletal disease
Polyarthritis due to Glässers disease in gilt litters
Polyarthritis due to Glässers disease was diagnosed at Bristol University in four-week-old piglets showing non-specific signs including sudden onset malaise, huddling and shivering in seven piglets, part of a 60-strong herd comprising eight sows, weaned pigs and pre-weaned piglets from five litters.
Affected piglets were all born to gilts suggesting that they may not have provided adequate immunity to their piglets.
There was purulent material in all joints examined and Haemophilus parasuis was isolated from the lung and hock joint of one pig. The piglets responded well to treatment with antimicrobial treatment although new cases continued to be seen for a further two weeks.
Bacterial polyarthritis, meningitis and likely greasy pig disease in preweaned piglets
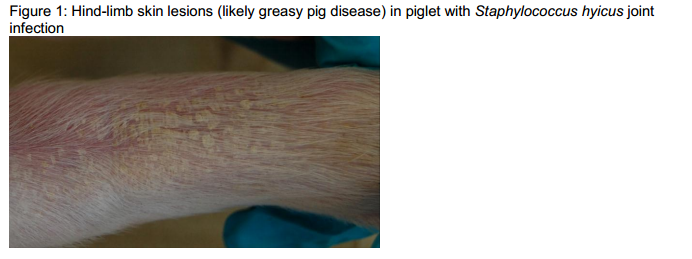
An 18-day-old piglet with meningitis-like signs and a nine-day-old piglet with swollen joints were euthanased and submitted to Camarthen to investigate the causes of both conditions.
The herd was experiencing an increased incidence of joint ill (approximately three-four per cent affected) in the farrowing house. Both conditions were reported to respond well to antimicrobial treatment. There was fibrinous exudate in several joints of both pigs and the meninges of both appeared congested.
Streptococcus suis type 14, a cause of polyarthritis, septicaemia and meningitis in piglets, was isolated from the brain and one joint of the older piglet.
Staphylococcus hyicus, the cause of greasy pig disease, was isolated from two joints from the younger piglet and this piglet did have some skin lesions on the hindlimbs (Figure 1) resembling greasy pig disease. Both pigs also had limb abrasions suggestive of floor trauma which may have allowed the staphylococcal infection in the younger piglet to enter.
Attention to colostral intake, improving hygiene and addressing any factors which could be damaging the skin, including an assessment of the flooring, were recommended.
Erysipelas strongly suspected on a smallholder unit
A group of four Saddleback pigs, aged approximately 15-weeks-old, developed swollen joints and pyrexia over a one to two week-period. One had also been inappetent and had lost condition. A blood sample submitted to Shrewsbury from one of these pigs had a high erysipelas antibody titre, of 1/20480.
The pigs had not been vaccinated for erysipelas, and therefore a titre of this magnitude together with the clinical signs reported was considered to be strongly suggestive of erysipelas. Confirmation of the diagnosis requires the organism to be isolated in culture, or seroconversion to be detected by paired serology.
Skin Disease
Staphylococcal skin disease causes skin lesions resembling pig pox
Three 18-week-old housed pigs were euthanased and submitted as part of a continuing investigation into porcine circovirus two-associated disease (PCVAD) which had begun about five weeks earlier. Clinical signs included pallor, coughing, wasting and 15 per cent mortality.
Approximately 200 of 880 pigs were affected over the five-week period and were from a single source. PCVAD had been diagnosed in a previous submission and the virus was a PCV2b typical of previous viruses and not the PCV2b variant.
The pigs were vaccinated for Mycoplasma hyopneumoniae and should have been PCV2-vaccinated but there was uncertainty about compliance with the vaccination schedule. Two of the pigs had multifocal circular raised lesions over the ear pinnae, dorsal neck, body and upper legs measuring three mm to three cm with pale peripheries and darker scabbed centres.
Lesions in the more severely affected pig are illustrated in figure 2. Pig pox was considered a possible differential but pox virus was not detected by electron microscopy and histopathology was consistent with a primary bacterial cause, similar to juvenile impetigo, the pathogenesis of which involves staphylococcal exfoliative toxins.
The pustules were more discrete and the acanthocytes were more numerous than is usual in Staphylococcus hyicus (greasy pig)-associated lesions. Staphylococcus lentus was isolated rather than S. hyicus; this organism is not usually associated with skin disease in pigs and is of doubtful clinical significance.