How to recognise poisoning
This is never easy because of the myriad of potentially toxic substances likely to be present on a farm, however always look for the most common and obvious first.
A poison may only affect an individual animal within a group because it was the only one inadvertently exposed to it. For example a toxic dose of medicine was administered by mistake.
Similarly most or all the pigs in a pen, a number of pens or a complete building may be affected, indicating a much wider exposure. Finally a complete herd may be affected - invariably associated with a common feed, water source or airborne pollution.
Step 1- Study the history carefully
Consult with your veterinarian
- Is the onset rapid - usually within 48 hours? If so, are a number of pigs affected?
- Is only a particular age group affected, for example gilts, sows, sucking piglets? If so, what is common to the group?
- What routines, medicines, management procedures have been applied to the group recently?
- Is a particular area of the farm or a number of pens affected? If so are there any common factors?
- Does the appearance of the condition coincide with the introduction of a new batch of feed or feed ingredients, a change in water or other local change?
Step 2 - Clinical signs
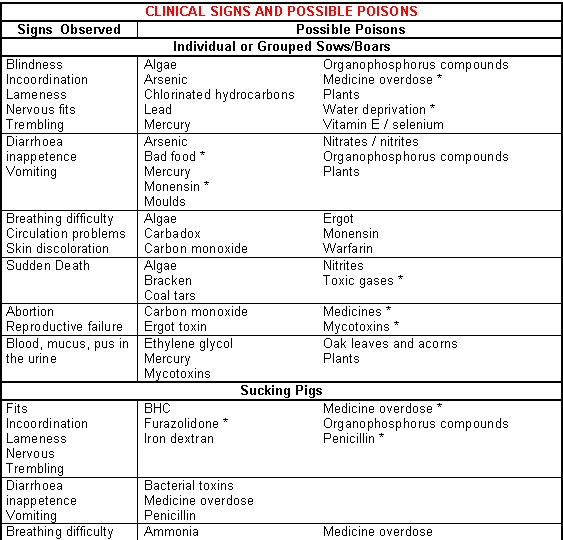
- List the clinical signs. (See Fig.13-1 and Fig.13-2).
- Common features of poisoning include:
- Rapid onset - (There are however exceptions depending on the dose level and period of exposure).
- A defined group of pigs affected.
- A number of pigs with identical clinical signs.
- Not a recognisable disease.
- Rectal temperatures are usually normal.
Clinical signs of different poisons
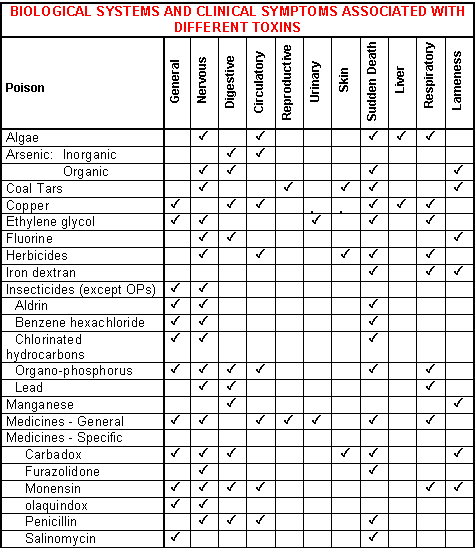
A broad outline of how different poisons affect different systems of the pig is given in Fig.13-1.
This can be used to help identify possible causes, particularly if used in conjunction with Fig.13-2. Specific systems of the body may be affected and develop the following signs:
Circulatory system
- Anaemia.
- Cyanosis (blue discoloration of skin).
- Increased respiration.
- Jaundice.
- Haemorrhage.
Digestive system
- Abdominal pain.
- Diarrhoea - with or without haemorrhage.
- Rectal prolapse.
- Salivation.
- Vomiting.
General effects
- Generalised malaise.
- Reduced feed intake or complete inappetence.
- Reduced growth.
Locomotor system
- Abnormal gait.
- Ataxia.
- Incoordination.
- Lameness.
Nervous system
- Blindness.
- Excitation.
- Fits.
- Incoordination.
- Spasmodic movements.
Reproductive system
- Abnormal oestrus.
- Swollen vulva.
- Abortion.
- Embryo reabsorption.
- Failure of fertilisation.
Respiratory system
- Coughing.
- Difficulty breathing.
- Pneumonia (found at post-mortem examination).
- Sneezing, nasal discharge.
Skin
- Colour.
- Haemorrhage.
- Irritation.
- Vesicles.
Urinary system
- Blood in the urine.
- Cystitis / pyelonephritis (found at post-mortem examination).
- Excess mineral deposits (found at post-mortem examination or in the urine).
- Pus.
Step 3 - Post-mortem examinations and records of mortality
Post mortem examinations may assist in differentiating between a specific disease and toxic conditions. Samples from tissues are probably required for further laboratory tests. The number of deaths and whether they are sudden or after a short or prolonged illness may characterise certain poisons.
The information assessed from steps 1 to 3 will raise a suspicion of poisoning.
Step 4 - Identify the possible sources of the poison
- List the chemicals on the farm - sprays, pesticides etc.
- List the medicines on the farm.
- What injections have been given?
- Are rodenticides used and available?
- Are parasecticides used?
- Could any sources of feed be suspected?
- Is there evidence of spoiled or mouldy feed or mould in the feed delivery system?
- Consider water, bedding and other environmental contaminants.
- Are sprays / disinfectants used.
- In out-door herds consider plants, water and environmental contaminants.
- Do any of the signs fit into Fig.13-1 or Fig.13-2?
Step 5 - Identify the toxin
Use Fig.13-1 to identify the potential toxin or toxins, together with the history and symptoms.
Step 6 - Read about the poison
Refer to the poison in the text and administer treatments in conjunction with veterinarian advice.
Step 7 - Confirm the poison
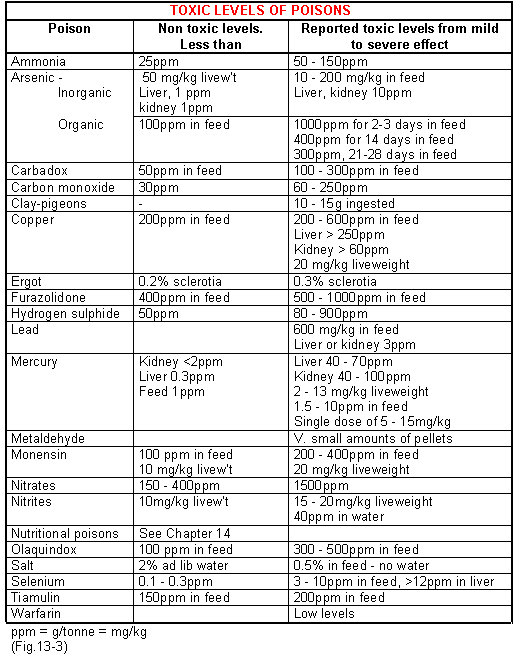
Refer samples to a lab for confirmation. (Fig.13-3).